Can You Grade Canine Mast Cell Tumors on Cytology???
A primer on the shifting landscape of MCT diagnostics and management
A bold new frontier in MCT diagnosis…
For many years, the approach to canine mast cell tumors was simple: Stick a needle in the mass, look at cytology under the microscope to confirm the baseline diagnosis of MCT. Then, the universal conventional wisdom went, the gold standard for next steps was to send off a biopsy for histopathologic grading to predict outcome and how aggressive the treatment protocol should be.
However, clinical pathologists and oncologists have long known some neoplastic mast cells look pretty bland under the microscope, while others are ugly and poorly-differentiated. The original 3-tier MCT grading system1 relied on primarily histologic architecture features that could not be seen on FNA cytology, but a newer 2-tier system2 based primarily on the individual cellular features of a biopsy has gained traction. Based on this, multiple recent studies have investigated one of the Holy Grails for veterinary oncology: cytologic grading criteria for canine mast cell tumors.
On top of this, a recently released drug (Stelfonta by Virbac3) complicates the diagnostic landscape as it may damage tissue after intra-tumoral injection and interfere with accurate histopathologic grading, creating a desire to grade MCTs cytologically before administering the agent. The efficacy of the drug may also differ between cytologically low-grade and high-grade MCTs4.
AUTHOR’S NOTE: I do not have any affiliation with Virbac or the development/sales of Stelfonta, and do not advocate for or against using it. I only mention it here because of its connection to MCT cytology grading, and will only discuss it in the context of regulatory and peer-reviewed publications. For clinical questions about Stelfonta, consult with a board-certified veterinary oncologist.
All of this is to say that the landscape for diagnosing and managing MCT just got a lot more complex (and confusing!) In this article, you will learn the following:
What cytologic grading systems have been published and their specific grading criteria
A comparison of the cytology grading schemes amongst each other, with an analysis of similarities, differences, and practical points
How cytology grading compares to traditional biopsy histopathology grading for MCT and clinical outcome
Competing Cytologic Grading Schemes
The first proposal for cytologic grading of canine mast cell tumors came in a 2011 letter to the editor in the journal Veterinary Clinical Pathology, where the authors elegantly made the case and presciently predicted some of the future pitfalls: 5
“In our diagnostic service, we have frequently observed certain discrepancies between cytologic and final histologic grading systems, especially in moderately differentiated and well-differentiated MCT variants. Grading a MCT with poor differentiation poses no difficulty, as major malignant criteria are invariably present; presumably there would be good correlation between cytologic and histologic grades in this category. Because cytologic evaluation of MCTs is performed during the initial diagnosis before chemotherapy in most cases – or even during a more radical surgical procedure, a reliable cytologic grading system is highly desirable”
This article provoked much discussion among clinical pathologists, but nothing changed for five years, until three studies using different cytologic criteria for grading MCT were published the same year in 2016! It is worth digging into these studies individually to discuss the methods, findings and their limitations.
Camus et al: “Cytologic Criteria for Mast Cell Tumor Grading in Dogs With Evaluation of Clinical Outcome”
The most robust of the three studies, in my opinion, is Camus et al (2016)6. It was the largest of the three with 152 MCTs from 150 dogs, versus 141 MCT in Hergt et al and 50 in Scarpa et al. More important than this size difference, Camus et al was the only study of the three that was prospective and compared their cytology and histopathology grading systems to clinical outcome over a two-year period. Other elements of their methodology that added to the strength of the study include using statistical methods to evaluate which of many proposed cytologic features were more discriminatory between high and low grade MCTs (rather than sampling copying the 2-tier histopathology system), and testing this system by blinded evaluation of both cytology and biopsy specimens by three board-certified anatomic and clinical pathologists at multiple institutions.
Patients in this study were required to have paired cytology and biopsy samples. All cytology slides were stained with an alcohol-based Wright’s stain (not Diff-Quick, which is important later!) Biopsies were evaluated by both 2-tier and 3-tier MCT grading systems mentioned above, as well as assessed for additional pathologic parameters and surgical margins. Clinical outcome data was available for 137/150 dogs (91.3%).
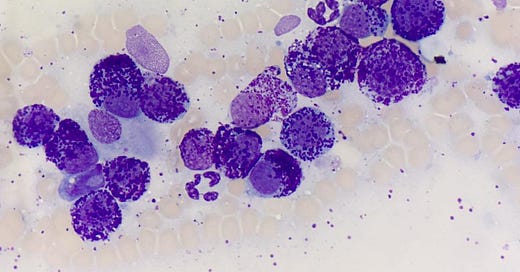
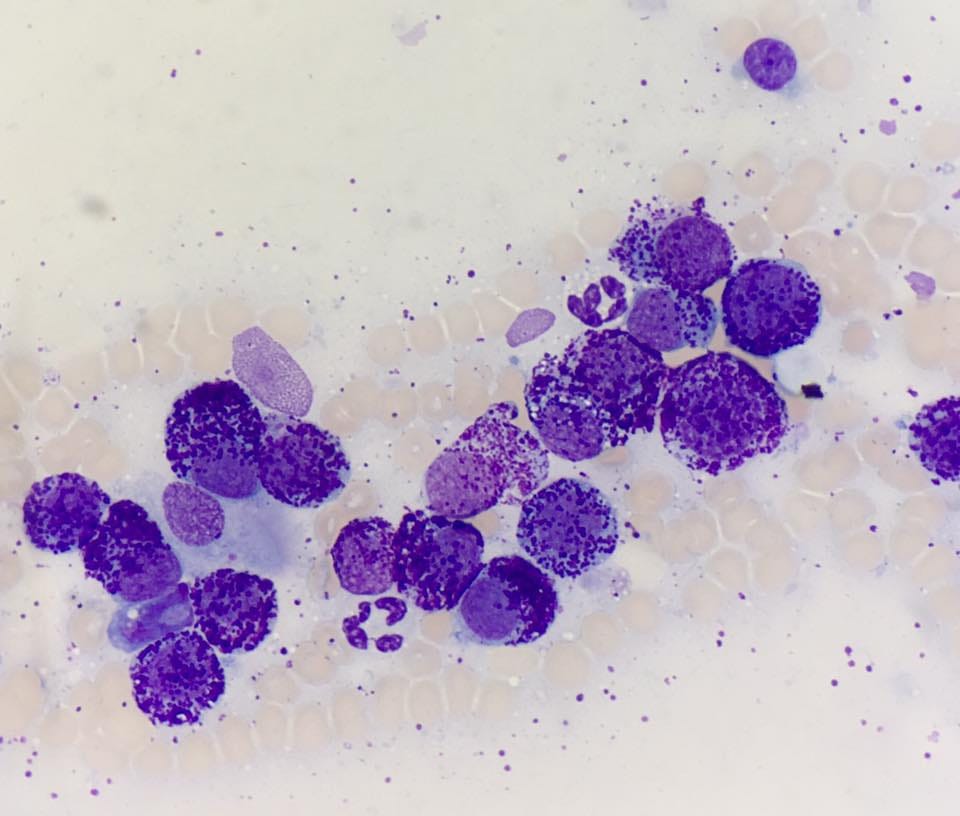
After performing ANOVA and statistical analyses, the authors created the two-tier cytologic grading system illustrated above. In brief, this grading scheme is a two-pronged test for whether or not a MCT is high grade. The first prong is assessing whether mast cells are uniformly poorly-granulated. The uniform part is key: If some cells lack granules but there is a mix of moderate to heavily-granulated cells, it fails this first test. The other important call-out is that this study was performed on alcohol-based Wright’s stain, which picks up metachromic granules very well. In contrast, water-based rapid stains like Diff-Quick often have a harder time staining these granules (see the example below). Therefore, this part of the grading system has not been evaluated using aqueous rapid stains, and I would not recommend relying on it for any slides that have not been stained with Wright’s stain.

The second prong of the Camus test is more straightforward. If at least two of the following four criteria are present, the MCT is considered cytologic high-grade:
Mitotic figures (any identified)
Nuclear pleomorphism (presence of non-round shapes)
Binucleation or cells with 3+ nuclei (any identified)
Significant anisokaryosis (>50% variation in nuclear size)
To see an example of this test in action, evaluate these two fields from a canine MCT cytology slide:

So now that we have a handle on how to apply these grading criteria, how does the cytology score compare to the current gold standard (biopsy grade)? In this case, the sensitivity of this system for high grade MCT was 88.2%, while the specificity was 94.8%. Factoring in the distribution of MCT grade prevalence in this study, that means that a negative test was 98.5% to be a true low-grade MCT on biopsy, but a high-grade cytologic MCT had only a 68.2% probability it was high-grade on biopsy. Therefore, the risk of a “false positive” determination of high-grade MCT is more likely than the risk of a false negative (calling something low-grade on cytology that is actually high-grade on biopsy). This highlights the importance of following up a preliminary MCT grade based on cytology with a biopsy grade.
The most important question with any grading system is whether or not it predicts clinical outcome. Or, said another way, what does finding a MCT meets the criteria for high-grade actually tell me about the prognosis? In this study, patients with high-grade MCTs had significantly shorter survival times, whether it was based on cytology or biopsy (see below). The median survival time (MST) for dogs with cytologic low-grade tumors was 562 days vs 364.6 for cytologic high-grade MCT. Dogs with cytologic-high grade MCT had a mortality hazard ratio of 25.0, meaning they were 25 times more likely to die during the study period than patients with a low-grade MCT by cytology!

Alternative Grading Systems
As I mentioned earlier, there are several other studies that have evaluated cytology grading systems for MCT. We will spend less time on them because they have larger methodological weaknesses, are less practical, and/or have not been as widely embraced as the Camus et al system.
In Hergt et al7, 141 mast cell tumors diagnosed on cytology with paired biopsy specimens were included. The cytology slides, which were originally stained with alcohol-based Giemsa stain, were de-stained with ethanol and re-stained with hematoxylin & eosin (H&E), the stain routinely used for histology. Samples were reviewed by a single pathologist. The 2-tier histopathology grading criteria for MCT were directly applied, such that a case was considered high-grade if the cytology contained one or more of the following: (1) 7+ mitotic figures/10 high powered fields, (2) 3+ multinucleate cells (3 or more nuclei, NOT binucleated) per 10 hpf, (3) 3+ bizarre nuclei /10 HPF, or (4) presence of karyomegaly (any). In this study, the sensitivity was 86.8%, specificity was 97.1%; 5 cases that were high-grade on biopsy were incorrectly called low-grade on cytology.
Finally, Scarpa et al8 is the smallest of the three 2016 studies at only 50 cases, and methodologically was a bit of a hybrid of the previous two. They used the two-tier histopathology grading criteria to Wright-stained cytology slides without re-staining with H&E. Their diagnostic performance was similar to the others, with sensitivity of 84.6%, specificity of 97.3%, and an overall accuracy of 94%. 2 high-grade tumors on biopsy were called low-grade on cytology.
Limitations and Controversies
How accurate is accurate?
None of these systems has perfect diagnostic accuracy. This is not surprising in the world of human or veterinary oncology grading systems—We are always trying to standardize and improve methods of diagnosing and sub-classifying cancer, but tumors are biologically complex, and don’t always follow the rules. In general, the Camus et al study had a higher risk of a false-positive diagnosis of high-grade status, with almost non-existent risk of false negative, so this may represent the better screening test. The other two systems that adhere closer to the 2-tier histologic grading system had few false-positives, but missed some cases of high-grade tumors on cytology.
Staining!
I mentioned it in the section of about the Camus study, but it bears repeating: The specific performance of any of these studies is critically dependent on what stain you are using. The most common stain in practice is Diff-Quik type stain, yet it is inappropriate to assess mast cell granularity with that stain. Furthermore, the Hergt study evaluated the H&E stain used on biopsy tissues, which is not used in practice or most clinical pathology labs, and as such, is not very practical or applicable.
Location, location, location!
There are separate histopathologic grading schemes for MCTs completely surrounded by fat (subcutaneous MCT) compared to more superficial cutaneous MCTs. The existing cytology grading schemes above sidestep this issue by only applying them to truly cutaneous MCT. However, while you sometimes may be able to tell an obvious cutaneous MCT that is within the dermis/epidermis from a deep MCT covered by fat and tissue on palpation, in practice this be can be challenging. The problem in the new era of Stelfonta is this: you often need a histopathologic biopsy to differentiate a cutaneous from a subcutaneous MCT, creating a chicken-and-egg problem whereby you have to make the decision about grading the tumor cytologically and administering a drug that precludes follow-up biopsy before you obtain histopathology.
Lastly, none of the grading systems in this post apply to mast cell tumors outside the skin (ie. visceral, organ-based, non-skin mucosa, etc) or to other species, like cats or horses.
Final thoughts
In the end, based on the evidence we have today, it is indeed possible to grade MCTs on cytology. In my opinion, the cytologic grade—when applied correctly—can be a useful piece of diagnostic and prognostic information, but it does not replace a histopathologic biopsy, ancillary MCT prognostic tests (such as IHC or PCR), or your clinical impression. Furthermore, the specific cytologic features evaluated and grading scheme performance vary by what system and study you’re talking about. There is no simple right or wrong answer to the question of whether or not to grade them—There are enough limitations and pitfalls that any veterinarian needs to be aware of and make sure they understand before attempting to grade, or they could end up misinterpreting the data and going down the wrong clinical path. These grading criteria are also best-applied by well-trained pathologists, rather than trying to parse the morphologic description yourself to figure out the grade. I would strongly recommend you talk with your veterinary pathologist about any patient-specific questions regarding MCT cytology grading after receiving a report, or ideally before submitting the case.
Patnaik AK, Ehler WJ, MacEwen EG. Canine cutaneous mast cell tumor: morphologic grading and survival time in 83 dogs. Vet Pathol. 1984 Sep;21(5):469-74. https://pubmed.ncbi.nlm.nih.gov/6435301/
Kiupel M, et al. Proposal of a 2-tier histologic grading system for canine cutaneous mast cell tumors to more accurately predict biological behavior. Vet Pathol. 2011 Jan;48(1):147-55. https://pubmed.ncbi.nlm.nih.gov/21062911/
“FDA Approves First Intratumoral Injection to Treat Non-Metastatic Mast Cell Tumors in Dogs.” https://www.fda.gov/animal-veterinary/cvm-updates/fda-approves-first-intratumoral-injection-treat-non-metastatic-mast-cell-tumors-dogs
Brown GK, et al. Intratumoural Treatment of 18 Cytologically Diagnosed Canine High-Grade Mast Cell Tumours With Tigilanol Tiglate. Front Vet Sci. 2021 Aug 27;8:675804. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8429927/
Pedraza F, Grandi F, Rocha NS. The need for cytologic/histologic correlation studies to establish a cytologic grading system for canine mast cell tumors in veterinary medicine. Veterinary Clinical Pathology, 2011;40:280-281. https://pubmed.ncbi.nlm.nih.gov/21884183/
Camus MS, et al. Cytologic Criteria for Mast Cell Tumor Grading in Dogs With Evaluation of Clinical Outcome. Vet Pathol. 2016 Nov;53(6):1117-1123. https://pubmed.ncbi.nlm.nih.gov/27034386/
Hergt F, von Bomhard W, Kent MS, et al. Use of a 2-tier histologic grading system for canine cutaneous mast cell tumors on cytology specimens. Vet Clin Pathol. 2016 Sep;45(3):477-83. https://pubmed.ncbi.nlm.nih.gov/27483044/
Scarpa F, Sabattini S, Bettini G. Cytological grading of canine cutaneous mast cell tumours. Vet Comp Oncol. 2016 Sep;14(3):245-51. doi: 10.1111/vco.12090. https://pubmed.ncbi.nlm.nih.gov/24717019/