Field Notes: October 2025
A roundup on AI, antibiotic resistance, screwworm, and digital pathology

Dear Readers,
I can’t believe it’s already October! This summer absolutely flew by with travel across the US, Canada, and Caribbean. Now the weather in Tampa is (finally) starting to cool down, which is a welcome relief from the sweltering heat of the last few months, especially for someone like me whose favorite season is autumn. Still, it is nowhere near as pretty in Florida as the vibrant fall foliage in upstate New York, as seen in the header image for this article.
One type of post that used to be more regular at All Science was a roundup of science news stories and research papers. Over the last year or so I have shifted focus more to big picture commentary on controversial issues in veterinary medicine and the broader culture. However, I’ve been meaning to return to this type of quick-hit capsule summary, so I’m introducing a new-ish format called “Field Notes” that will be a regular feature. I’d appreciate any feedback on the structure, content, and frequency of this type of post. Without further ado, here is a selection of interesting articles I’ve been reading (and one I was involved with writing).
—Eric
Digital cytology validation & best practice guidelines
A big part of my career has involved digital pathology, both in building companies like CytoVetStat and Lacuna Diagnostics, and reading virtual slides remotely as a contractor for several labs, and I’ve previously written about this on All Science (see below). For the past two years, I have been working with a large, multi-institutional group of pathologists from academia, pharma, and private diagnostic companies to write guidelines for the validation and implementation of this technology.
The 2025 ASVCP Digital Cytopathology Quality Guidelines sets the foundation for ensuring that digital slide interpretation in veterinary medicine meets the same standards of accuracy, reliability, and patient safety as traditional light microscopy. This document provides a comprehensive roadmap for laboratories and clinicians adopting digital cytology—covering every step from how samples are prepared and scanned to how images are validated, interpreted, and reported. The guidelines also detail how to train staff and pathologists in digital systems, manage out-of-focus or incomplete scans, and communicate transparently about image limitations or preliminary findings.
You can find the white paper on the ASVCP website here, and it will soon be published in the journal Veterinary Clinical Pathology.
Screwworm moves closer to the US
JAVMA News recently reported that there were over 5,000 cases of screwworm reported in Mexico in August, a >50% increase from the month prior, and one case was detected just 70 miles from the Texas border. For those who aren’t vets, you might be wondering what the hell a “screwworm” is and why we’re talking about something so gross. Well, the New World Screwworm (NWS) or Cochliomyia hominivorax is a parasitic blowfly that has a terrifying lifecycle: Its larvae feed on living flesh 😱 As you can imagine, this can cause serious injury and even death to those it feeds on, which includes farm animals, pets, wildlife, and occasionally even people.
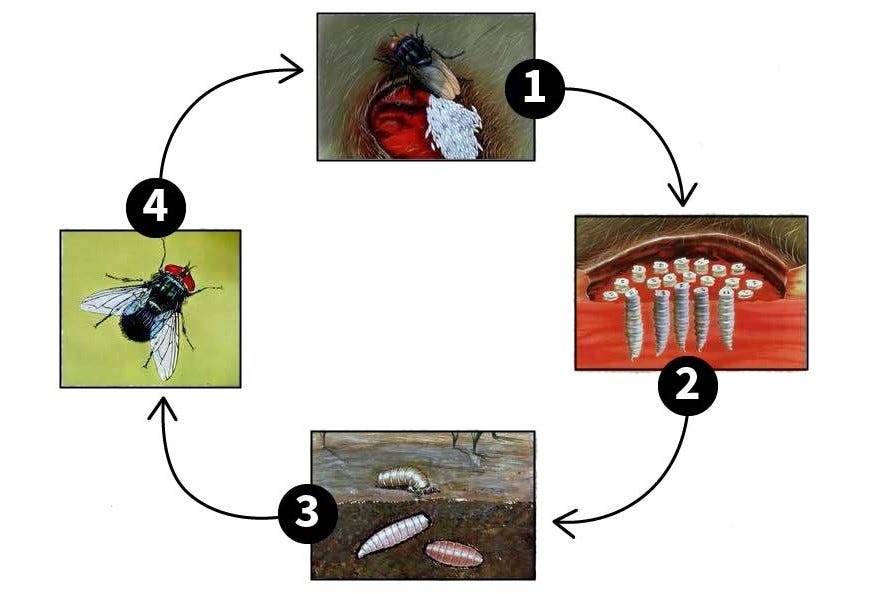
The United States eradicated NWS in 1966 using sterilized male flies that break the lifecycle. Since then, the USDA and veterinarians across the country have been vigilant to prevent this parasite from re-establishing itself in the US, by restricting and inspecting animals that cross the border as well as monitoring traps and other detection systems.
NWS is endemic in much of South America and the Caribbean, although Mexico and Central America had been free of screwworm until recently, when COVID-19 disrupted sterile insect distribution in Panama. The fly resurfaced in Mexico in 2024 and was able to rapidly spread north, as a single female NWS can fly hundreds of kilometers and lay 3,000 eggs in her lifetime.
Veterinarians across the US should be on the lookout for potential screwworm lesions and immediately report any cases to their state veterinarian and any other relevant public health agencies. Pet owners should immediately contact a vet if they notice maggots on their animals (though hopefully you would do that even without this outbreak!) Finally, state and federal public health agencies are going to have to collaborate with Mexico and other Central American countries to push back NWS. As assistant state veterinarian in Texas Dr. T.R. Lansford aptly put it:
“A problem in Mexico is a problem for the United States […] That’s why surveillance and awareness are critical, especially along the border but really throughout the country.”
Antibiotic-resistant bacteria can spread from pets to people
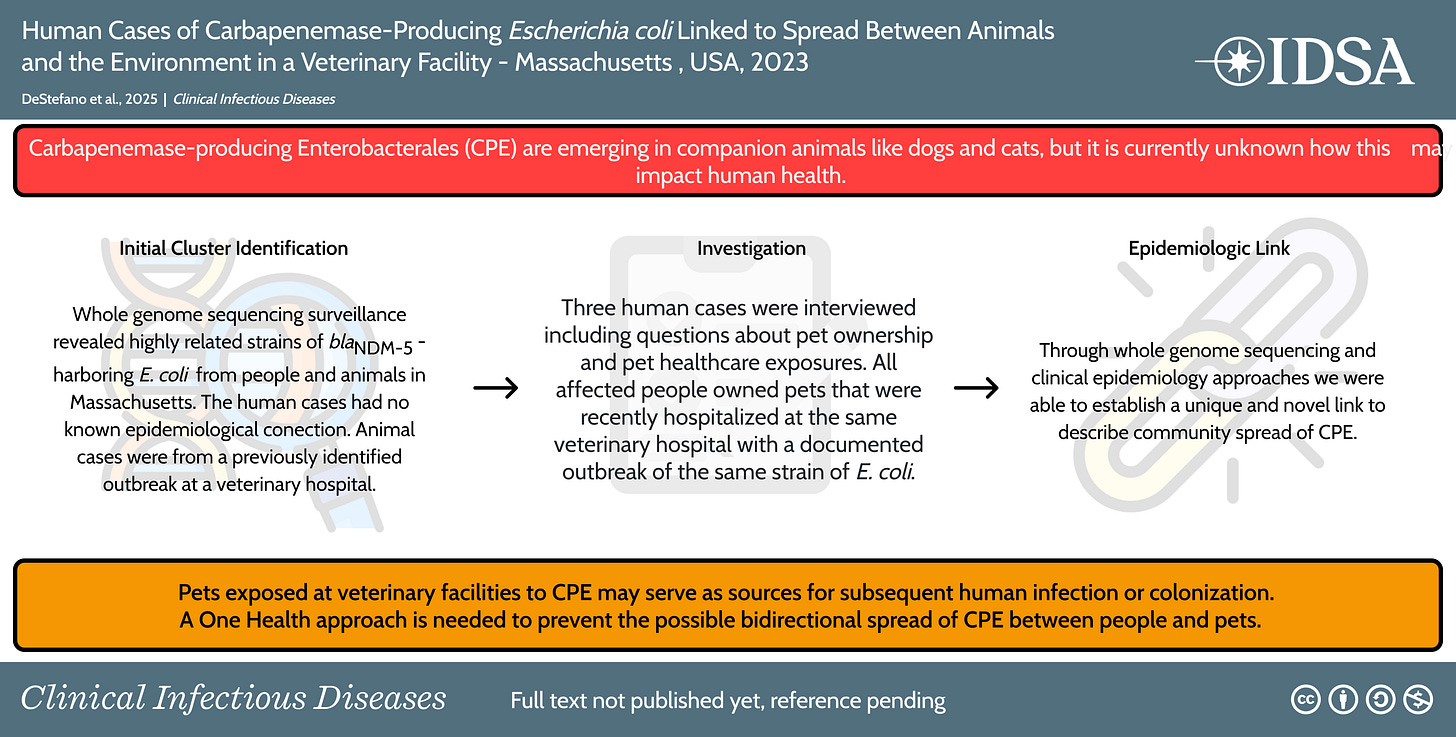
In another One Health story, researchers in Massachusetts1 recently discovered that a dangerous type of antibiotic-resistant bacteria that originated in pets was transmitted to three people2 in the nearby area. Originally, multiple cats and dogs at a veterinary hospital in Worcester, MA were diagnosed with Carbapenemase-producing E. coli. This type of bacteria has a gene that makes it immune to multiple different types of drugs, which can be transmitted to other bacteria.
The researchers were able to connect the animal cases to the human ones when they sequenced the bacterial genomes and found they were almost identical. Though the people had never met each other and an epidemiological investigation did not initially find any links, it turned out all had taken pets to the veterinary hospital that experienced the outbreak. The findings are summarized in the graphical abstract below:
This study is an outstanding example of collaboration between vets and public health officials that highlights the potential risk of transmitting multi-resistant bacteria from pets to owners. Veterinarians are becoming more aware of the need for antimicrobial stewardship—essentially changing drug prescribing habits to blunt the spread of these superbugs. So next time you are frustrated that your vet says “I don’t think your pet needs an antibiotic,” remember stories like this.
PS: Thanks to
for bringing my attention to this one!AI isn’t replacing radiologists (yet)
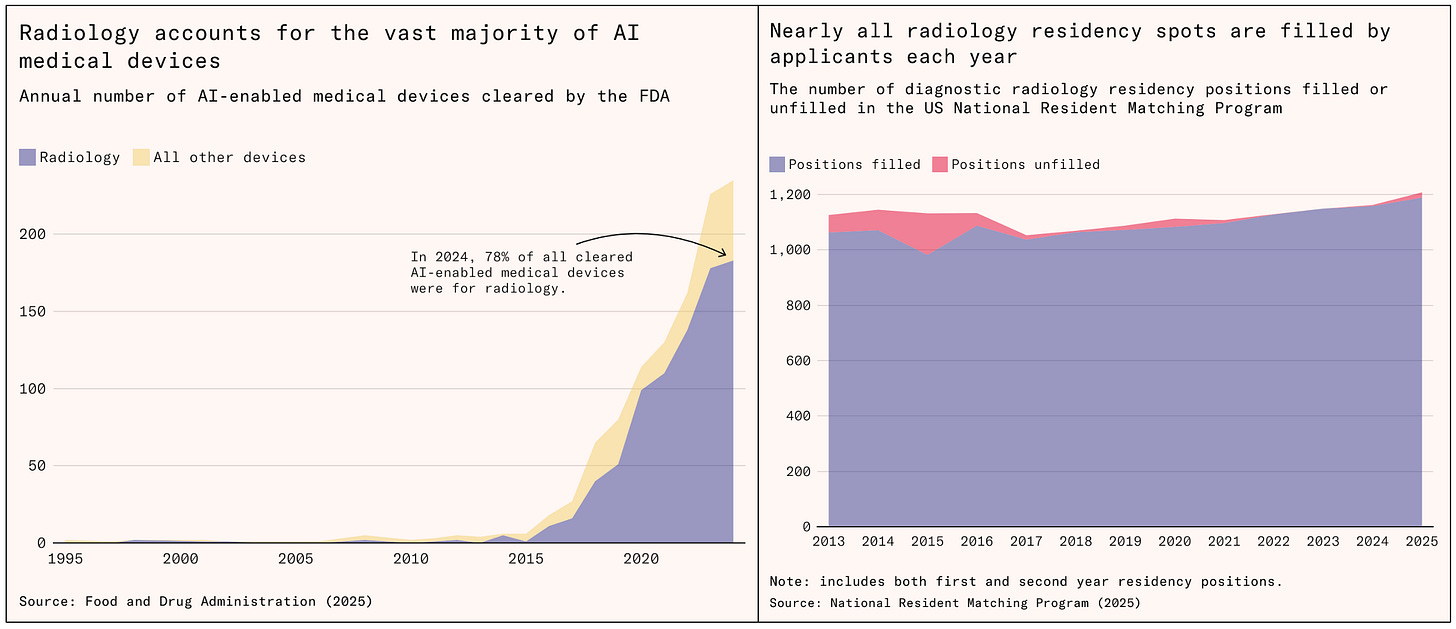
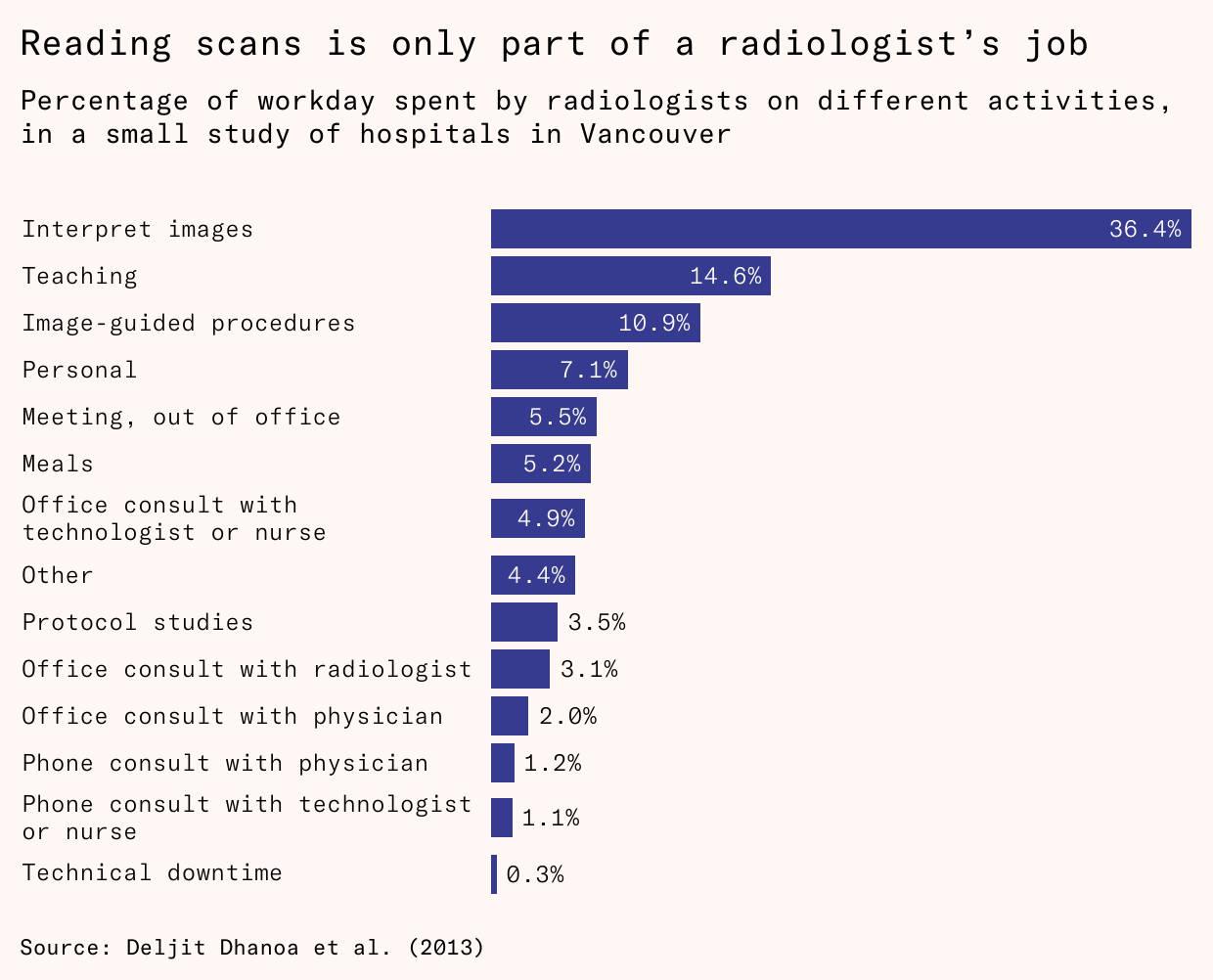
Finally, I wanted to bring attention to this excellent post on the Substack Understanding AI. It explores the use of AI in diagnostic imaging and dives into the reasons why it has not made a significant impact on the demand for radiologists. There are lots of reasons, but the big ones are these:
Three things explain this. First, while models beat humans on benchmarks, the standardized tests designed to measure AI performance, they struggle to replicate this performance in hospital conditions. Most tools can only diagnose abnormalities that are common in training data, and models often don’t work as well outside of their test conditions. Second, attempts to give models more tasks have run into legal hurdles: regulators and medical insurers so far are reluctant to approve or cover fully autonomous radiology models. Third, even when they do diagnose accurately, models replace only a small share of a radiologist’s job. Human radiologists spend a minority of their time on diagnostics and the majority on other activities, like talking to patients and fellow clinicians.
I have been warning about the mismatch between excellent performance of AI models on medical imaging tasks in studies versus real world settings (for example, this recent post on EKGs). There are also complex insurance and liability concerns. Finally, there’s the fact that better efficiency on some tasks can actually increase the overall work burden, as we’ve seen with clinical chemistry and hematology analyzers in diagnostic labs.
The whole article is excellent and worth reading for a reality check against the hype of AI taking over human diagnosticians 👇
Alright, that’s it for the inaugural edition of “Field Notes,” I hope you found something useful in it! Let me know what you think ahead of the next edition in a few weeks
The lead author Dr. Ian DeStefano is a WesternU grad who overlapped with me in school!
Two patients were older, a 79-year-old woman and a 63-year-old man, but one was a 23-year-old woman, reminding us that no one is immune from the risk of drug-resistant infections